**Note: Before reading this post about Polycystic Ovary Syndrome (PCOS) and eating disorders, it is highly recommended that you take a moment to read our page “Polycystic Ovary Syndrome” and check out our blog “6 Nutrition Tips for Ditching the PCOS Diet Culture”. If you are concerned that you may have PCOS be sure to check out our quiz “Do I Have PCOS” as well as contact your physician.**
You may have been hearing a lot about PCOS recently and wondering why it’s getting so much attention within the eating disorder community. Well, in the academic article “Increased Odds of Disordered Eating in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis” 8 studies were conducted consisting of 470 women with PCOS and 390 control subjects. The studies found that the odds of a woman with PCOS developing an eating disorder were higher than a woman without PCOS. This is partly because there is so much medical misinformation surrounding PCOS, making it difficult for women to navigate, much less understand, their condition. This is why we at Courage to Nourish have created this comprehensive guide explaining the unique hormone cycles associated with PCOS.
Medical Misinformation Surrounding PCOS
Women of all body types can be diagnosed with PCOS; however, according to the National Institute of Health (NIH) the majority of women with PCOS (38-88%) are in larger bodies. Due to the anti-fat bias in the medical field many women seeking help with this diagnosis are frequently given misinformation and unhelpful guidance from providers. Body size is not an indicator of health. And is not a prerequisite for a PCOS diagnosis as PCOS has more to do with hormones than body size.
Despite this, many medical providers still recommend their patients the following…
- Cut out food groups including gluten and dairy – there is no evidence suggesting this can help with PCOS management
- Cut out carbohydrates
- Decrease overall intake/start a restrictive diet/count calories
- Increase exercise/movement
**Please note that these recommendations are ill-advised, fatphobic, and not aimed at the core issue of PCOS which is hormone imbalance.**
If you have been given any of these recommendations by your provider, please reach out to a HAES aligned provider. You deserve better care. All of the recommendations above are, in a registered dietitian’s opinion, eating disorder behaviors.
Often doctors and other providers are recommending patients engage with eating disorder behaviors as a way to manage PCOS symptoms. However, not only are eating disorder behaviors problematic for many health, medical, and emotional reasons; but they exacerbate the PCOS symptoms an individual may be experiencing. None of these recommendations focus on the hormone imbalances that are occurring or offer solutions/treatments. In fact, many of these behaviors result in hormone imbalances for individuals. Seems kind of ridiculous right? We at Courage to Nourish find that this constant flow of misinformation from providers is downright negligent, irresponsible and dangerous.
PCOS and the Hormone Cycle
So, if the recommendations above are not the way to manage PCOS, what is? How does one with PCOS get to a place of hormone balance? Let’s backtrack to first review what happens in a woman’s hormone cycle. A woman’s hormone cycle can range from 21-40 days and is constantly shifting and changing throughout that range of days. On average we use 28 days as the typical range.
During the 21-40 days of the menstrual cycle, women have different nutrient requirements due to the fluctuation and shifts in reproductive hormones. Specifically, progesterone and estrogen. These hormones, despite being called reproductive/sex hormones, also influence body temperature, metabolism, hunger and food cravings. It’s no wonder why our intake, or lack thereof in certain situations, can influence our periods.
Two other hormones, Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) are important to note here. FSH does exactly as its name implies. It stimulates the follicles of the ovary to mature into eggs. LH assists with stimulating the release of eggs from the ovaries, ovulation, and the release of progesterone after ovulation.
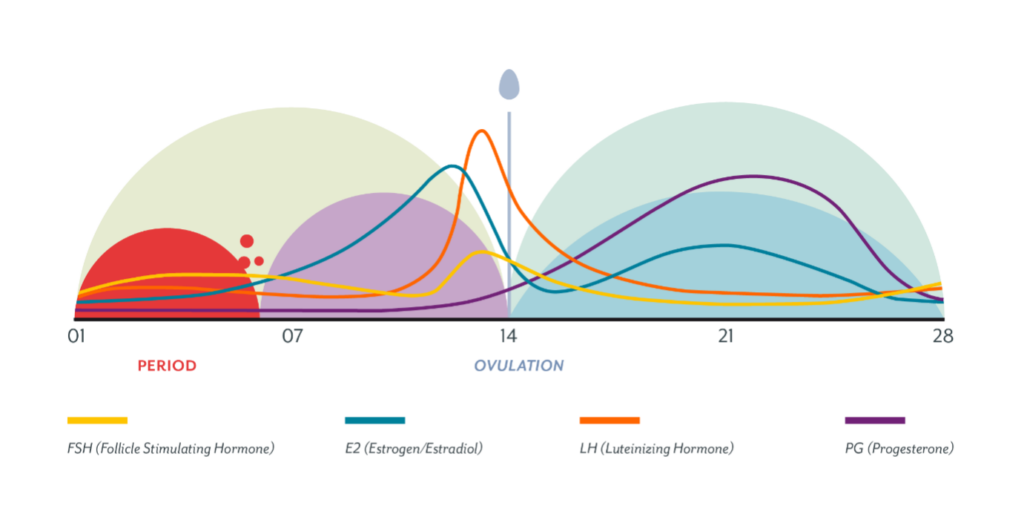
Refer to the diagram above for reference. The menstrual cycle is split into two phases, the follicular phase and the luteal phase. During the first half of the cycle, the follicular phase (you can remember Follicular, First), the period takes place. When a woman is menstruating, estrogen and progesterone levels are low. This is the time when the womb sheds its lining if it is not preparing to grow a fetus. Over the course of this phase, FSH levels will begin to rise. After the period is over, estrogen and LH begin to rise and ultimately peak right before ovulation (when an egg is released from the ovaries). Ovulation is the marker between the follicular phase and the luteal (you can remember Luteal, Last) phase. After ovulation, estrogen levels drop, while progesterone begins to rise. This is the only time in the cycle when it will surpass estrogen. Progesterone is helping prepare the womb for an egg to be fertilized there. If that does not occur then progesterone and estrogen fall again and we are back to the beginning of the cycle with a period.
You might ask the question again of why all of this matters. Well, putting PCOS aside, during the luteal phase when both estrogen and progesterone are high, there is an increase in metabolic rate. Meaning, that individuals need more energy and nutrition at this time. The degree of increase varies from person to person. As do many things with the human body; however, this often explains why women have a natural increase in cravings, intake, and hunger during this time. It is entirely normal to crave foods higher in carbohydrates and fats due to the fluctuation of hormones and the body’s biological need for more energy in the form of nutrition.
When looking at PCOS, this shift in hormones can be dramatically altered which disrupts the cycle. Typically, women with PCOS may have a higher LH to FSH ratio. Usually, LH is double that of FSH. An elevated LH causes the body to produce more testosterone. And lower FSH levels mean the follicles of the ovaries are not getting stimulated and are not releasing eggs, hence no ovulation. If you do not ovulate, the body cannot produce adequate amounts of progesterone. When hormones are imbalanced you can experience a lot of the symptoms such as excessive hair growth, hair loss, acne, irregular periods, absent periods, etc.
Final Thoughts on the PCOS and Hormone Cycle?
Thank you for reading this resource on the PCOS hormone cycle. So the question remains, what are those who have PCOS supposed to do? First, find yourself a HAES-aligned team of providers including a physician, dietitian, and therapist. If you’d like referrals please reach out to us or check out The Health at Every Size Healthcare Provider Listing. Secondly, stop blaming yourself. PCOS develops due to a mixture of environmental and genetic factors. Nothing an individual does or does not do will make them develop PCOS. Luckily, with the proper guidance those with PCOS can manage their symptoms and balance out their hormones. And that guidance does not include wacky diets, weird supplements or restrictions.
Contact Us
Courage to Nourish is a group of eating disorder specialized dietitians. We have in person locations in Alexandria, Virginia, Columbia, Maryland. and College Park, Maryland. We offer virtual services across the state of Virginia, Washington DC, Pennsylvania, and Colorado. We offer individual nutrition therapy. As well as support groups. We would love to guide you in building a better relationship with food.
Contact us for more information. And to schedule a discovery call. Also, sign up for our client or clinician newsletter!
Take one of our eating disorder quizzes:

